Trends
Avoiding the Anguish of Ill-Advised Automation
Automation ("tracks") is marketed to laboratories as the solution to most if not all of their problems. But when done poorly, it can actually causes more problems than it solves. Take this opportunity to learn the inefficiencies that may befall a laboratory that selects the wrong automation solution.
Avoiding the Anguish of Ill-Advised Automation
Labs, Look before you leap, part 2
Sten Westgard, MS
August 2017
 Automation is often represented as the ultimate boon, a mark of laboratory sophistication, the Holy Grail of operational efficiency. When a laboratory gets their track, they have arrived. They are now one of the big players. And if you search, you will find dozens of articles, white papers, and webinars extolling the benefits of automation, as well as superficial guidelines on how to select a track, and fuzzy, abstract discussions of the concept of automation (without getting into the gory grinding details that matter).
Automation is often represented as the ultimate boon, a mark of laboratory sophistication, the Holy Grail of operational efficiency. When a laboratory gets their track, they have arrived. They are now one of the big players. And if you search, you will find dozens of articles, white papers, and webinars extolling the benefits of automation, as well as superficial guidelines on how to select a track, and fuzzy, abstract discussions of the concept of automation (without getting into the gory grinding details that matter).
Here's the counter-point. There are times you should NOT get automation. There are labs that do NOT need automation. And just as there are instruments that deliver poor quality results, there are types of automation that don’t improve the laboratory, but actually make things WORSE.
In my years traveling the globe, I have seen the havoc that bad automation wreaks upon laboratories. For example:
- A laboratory where an entire automation line sits idle, because the speed of the track and the quality of the instruments turned out to be unacceptable. The line has to sit idle for years, while the hospital amortizes the huge expense of that mistake
- A laboratory where the track is so slow, they bought an entire duplicate set of instruments to operate for STAT and rapid testing. So they have twice the instrumentation costs and twice the labor needs – one set of staff to serve the STAT instruments, one set of staff to serve the automated instruments.
- A laboratory where the track does not actually track specimens – where once a specimen is sent down the line, there is no ability to know where it currently is. Subsequently, there are designated staff “chasers” who roam up and down the track trying to find samples that need add-on or reflex testing.
- And on and on...
I have seen too many laboratories that didn’t really examine the automation or the instrumentation before they made their decisions. And then they had to live with the regretful consequences for years – and so did the doctors and patients they serve.
If we generalize here are the top 5 reasons to avoid automation:
5. The Tube tie-up. There are lots of tube types. Some tracks and instruments can only accept one type. And therefore you must aliquot all incoming tubes of different sizes into the standard tube size of that track and instrument. Think all that extra aliquoting on the pre-track side still impacts your TAT? You bet it does.
[This tube issue can get even worse – there may be up to 11 different racks required by the different tubes in some tracks, while other tracks have a universal rack that can handle all tube types. Think that mean
4. The Dilution Dilemma. When specimens come in that have values in the high linear range, there are two problems that can creep up. If the instrument method has a narrow range, it can’t handle the high values, so it must auto-dilute, which doubles your turn-around time. Or, if no auto-dilution is present, you have to have a tech manually dilute the specimen. Will having staff manually handle dilutions negate some of the labor savings you’re supposed to get out of this track? You bet.
3. The One-way Runaway. Some tracks are uni-directional. Others go both ways: bi-directional. If your track only goes in one direction, once the specimen has been tested, it’s gone. Who has to bring it back down to earth to the front of the automation line when there are add-ons, reflexes, etc? Someone on your staff. Will the need to have specimen “chasers” dedicated to your line chew up even more of the labor savings you’re supposed to get out of this track? You bet.
2. The Sample-Splitting Headache. Some instrument systems can’t have specimens go through their chemistry instrument and then on to their immunoassay instrument. The chemistry instrument may actually make the specimen “dirty” – that is, contaminated by the sampling probe process in such a way as to interfere with any subsequent testing by other instruments. So this means – again- that prior to getting specimens on the line, you’ve got to split them so there’s a chemistry specimen and an immunoassay specimen. Who’s doing this extra aliquotting? Guess.
1. The Absence of Actual Analytical Quality. Automating poor quality instrumentation just makes bad results get reported more rapidly. At the heart of your track decision should be your instrument decision (which should take analytical quality into account). Don’t accept poor quality instruments just because they come with a “free track”. That free track isn’t really free – you’re paying for it, and when it doesn’t work correctly, and when the instruments deliver defective results, the clinicians and patients will pay for it, too.
Do you really want to brag to your patient that “we’ll get you the wrong result faster than ever before”?
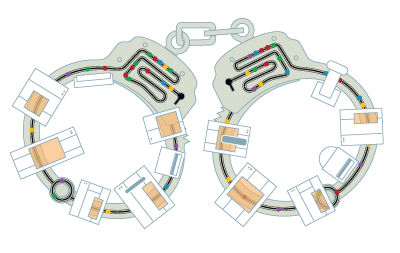
Remember, an automation line is “big iron” - heavy and hard to move. It’s like a battleship. Or a handcuff. Once you install it, you’re stuck with it for a long time, it takes a longer time to make a turn (change your mind) if you belatedly discover this thing isn’t working the way it’s supposed to.
Automation, when done right, can be a beautiful thing, a real productivity booster, staff shrinker, and result accelerator. But there are many ways you can get tracks – and instruments – wrong. Please, please be wary.